3D Mammography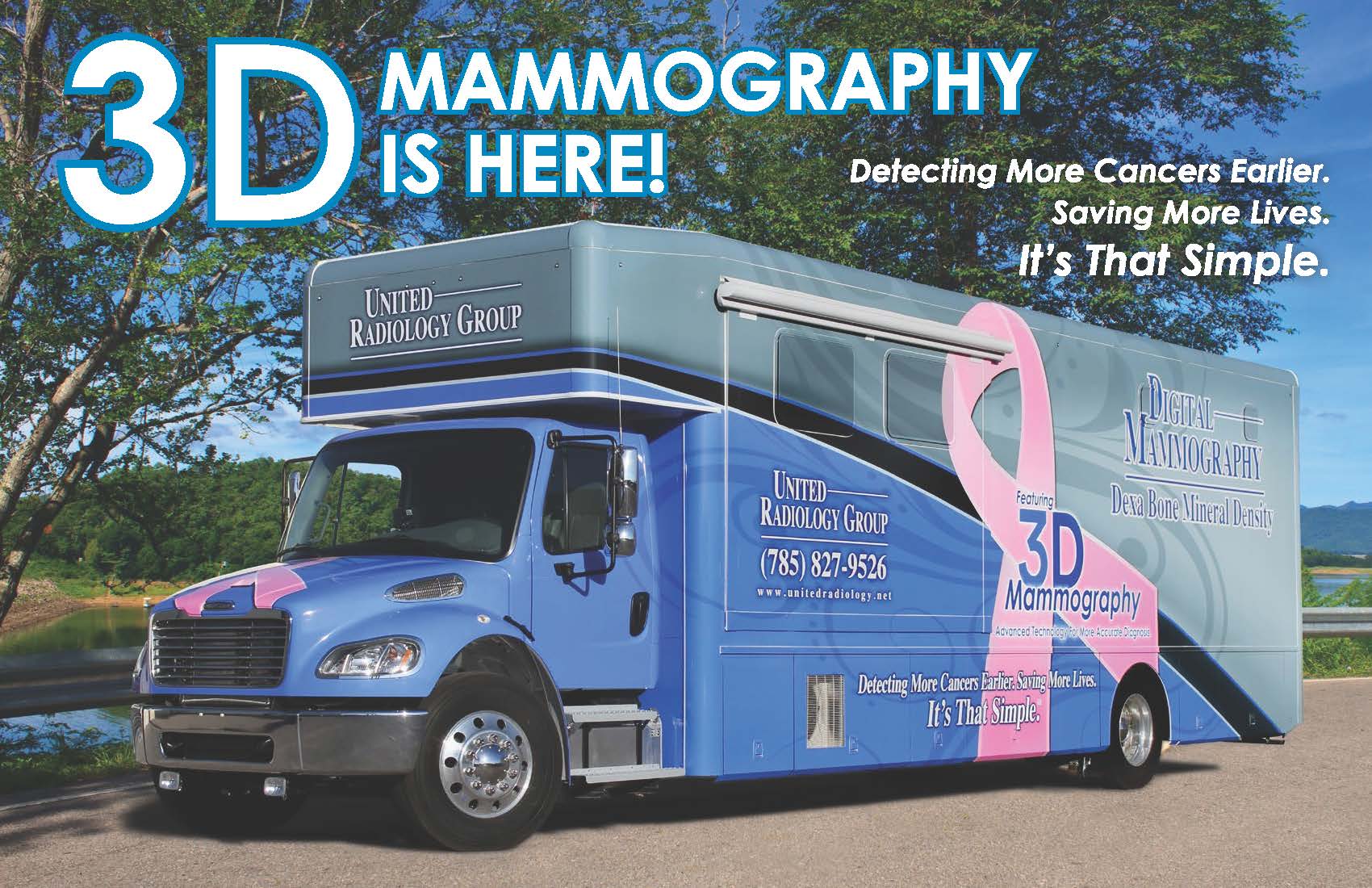
United Radiology Group has recently increased their services at TCLMH and other rural Kansas hospitals with the purchase of a new 3D mobile mammography coach. 3D mammography provides better quality exams, earlier breast cancer detection, and reduces unnecessary call backs by up to 40%. This new technology allows doctors to examine breast tissue layer by layer instead of a flat 2D image and detects 41% more invasive breast cancers. Women of all ages and breast densities benefit from this new service.
The new 3D Mammography coach features:
• Patient entrance
• Waiting area
• Reception/check-in desk
• Private changing rooms
• Wheelchair access door
• Private screening room
The mammography coach provides services once a month at TCLMH. Although most insurance plans cover the cost of 3D mammography, it’s important to check with your insurance provider first before scheduling. To obtain a 3D mammogram, please call the radiology department at (785)743-3411.
Patients must alert the technologist if they may be pregnant!
How is the procedure performed?
Mammography is performed on an outpatient basis.
During mammography, a specially qualified radiologic technologist will position your breast in the mammography unit. Your breast will be placed on a special platform and compressed with a paddle (often made of clear Plexiglas or other plastic). The technologist will gradually compress your breast.
Breast compression is necessary in order to:
- Even out the breast thickness so that all of the tissue can be visualized.
- Spread out the tissue so that small abnormalities are less likely to be obscured by overlying breast tissue.
- Allow the use of a lower x-ray dose since a thinner amount of breast tissue is being imaged.
- Hold the breast still in order to minimize blurring of the image caused by motion.
- Reduce x-ray scatter to increase sharpness of picture.
You will be asked to change positions between images. The routine views are a top-to-bottom view and an angled side view. The process will be repeated for the other breast.
